Collapse and unconsciousness in children
Fainting
(syncope, fainting)
is defined as a sudden short-term loss of consciousness caused by transient
acute cerebrovascular disorders on the background of autonomic
paroxysm.
Syncopal states (Video) are often considered as mild manifestations of vascular insufficiency, but it should be remembered that these conditions can be manifestations of severe diseases of the internal organs and are associated not only with pathology of the vascular system, but also with cardiac disorders, brain diseases, intoxications, etc.
Video.
Syncopal
states
Most
often in children syncope occurs due
to:
disorders of nervous regulation
of vascular tone (vagal,
vasovagal, orthostatic, sinocarotid, reflex, situational, hyperventilation
syndrome);
The vasovagal reflex consists of vasodilation (vaso) and bradycardia/asystole via the vagal nerve (vagal). These factors produce a fall in blood pressure, ultimately resulting in cerebral hypoperfusion and syncope.
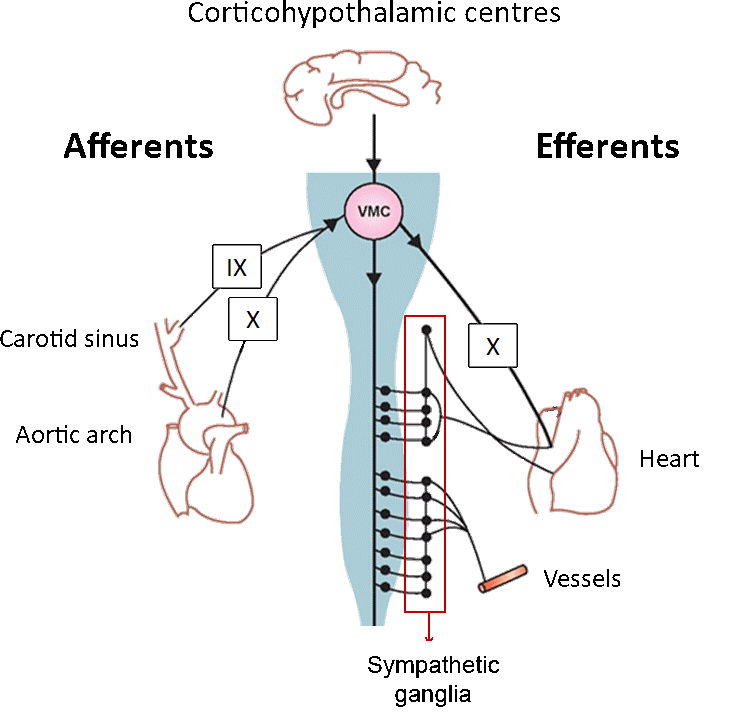
Figure.
A
schematic figure of the arterial baroreflex, with on the left the afferent
arm and on the right the efferent arm. IX
= glossopharyngeal nerve. X = vagal nerve
-
cardiac dysfunction in the presence of: bradyarrhythmias (atrio-ventricular block II-III degree with attacks of Morgan-Adams-Stokes, sinus weakness syndrome); tachyarrhythmias (paroxysmal tachycardia, atrial fibrillation); aortic defects; dyspnea-cyanotic attack of Fallot's tetrads with a sharp decrease in hemoglobin oxygen saturation;
-
disturbance of homeostasis (various intoxications, hypoglycemia, hypocalcemia, starvation);
-
cerebrovascular disorders;
-
bleeding;
-
reducing the oxygen content in the air.
Fainting
has the following successive stages of development (Video):
Video. Stages of development
-
disturbance of consciousness;
-
recovery.
Presyncopal period
(prodrome period)
may be characterized by deterioration of general condition,
discomfort, nausea, yawning, weakness in the legs, "darkening" in the eyes,
flickering "flies" in front of the eyes, noise or ringing in the ears,
dizziness, sweating, discomfort area of the heart or epigastrium. Sometimes, if
a child has time to sit or lie down, the attack may end there. In other cases,
fainting occurs instantly.
Syncopal state is
characterized by short-term loss of consciousness. The face is pale, covered
with sweat, the limbs are cold. The muscle tone is sharply reduced. Pulse is of
weak filling, BP is lowered, heart tones are weakened, heart rate and rhythm can
be various, breath is shallow. Pupils are dilated, reaction to light is
sluggish, skin reflexes are reduced. Tendon reflexes are normal. With a very
deep syncopal state (rarely) there may be short-term tonic convulsions. Loss of
consciousness usually lasts from a few seconds to one minute, rarely up to 2-5
minutes, in deep syncope - from a few minutes to 30-40
minutes.
In
the postsyncopal period,
weakness, pallor of the skin and mucous membranes, hypotension, yawning, deep
breathing is possible. Complete recovery and normalization of health lasts from
several minutes to several hours, depending on the severity of the
syncope.
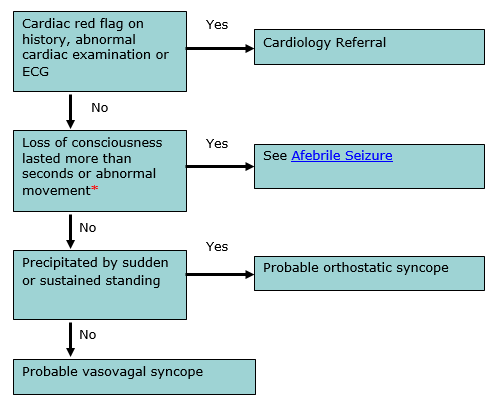
*There
may be brief tonic-clonic movements with vasovagal syncope
Figure.
Management
algorithm
-
put the child in a horizontal position with slightly raised legs and lowered head;
-
unbutton, loosen items of clothing that can compress the body;
-
provide access to fresh air or oxygen support, if necessary;
-
spray on the face with cold water, pat on the cheeks with a damp towel, napkin;
-
use irritating vasomotor agents – inhale the vapors of ammonia, vinegar;
-
rub the body, put hot-water-bottle;
-
in the absence of effect, in deep syncope it is recommended:
-
to enter subcutaneously 10% solution of caffeine benzoate
at a dose of 0.1 ml/year of
life or
-
to enter subcutaneously a solution of cordiamine at a dose of 0.1 ml/year of
life;
-
in the presence of low pressure should be administered intravenously (iv) 1% solution of mezaton (Phenylephrine) at a dose of 0.1 ml / year of life or iv drip on 5% glucose;
-
in case of hypoglycemia, inject 20-40% of glucose at a dose of 2 ml/kg;
-
with severe bradycardia, Morgan-Adams-Stokes attack, primary resuscitation measures are performed: closed heart massage; artificial lung ventilation if necessary; intravenous injection of 0.1% solution of atropine at a dose of 0.01 ml/kg;
-
after the onset of consciousness, the patient can not be immediately lifted, and should drink hot tea, calm down.
Collapse
is
a life-threatening acute vascular insufficiency
characterized
by a sharp decrease in vascular tone, decreased circulating blood volume, signs
of cerebral hypoxia, and suppression of vital functions.
The
main causes
of collapse in
children:
-
acute infections with severe course (intestinal infections with manifestations of toxic-exsiccosis, respiratory infections with neurotoxicosis, complicated pneumonia, pyelonephritis);
-
acute hypovolemic conditions (bleeding, dehydration);
-
acute adrenal insufficiency;
-
reduction of cardiac output (arrhythmias, cardiac tamponade);
-
overdose of antihypertensive drugs, poisoning by drugs, sedatives;
-
severe injuries;
-
action of physical factors, such as high temperature (heat stroke, overheating);
-
during puberty, especially in girls, orthostatic, emotional collapse is possible;
-
lack of oxygen in the inhaled air in the highlands (hypoxic collapse).
In
fact, the collapse in the expanded form is an acute circulatory disorder with
hypotension. According to the pathogenesis of collapse
there
are:
-
sympathicotonic, when arteriole spasm, centralization of blood circulation and, as a compensatory reaction, the release of catecholamines into the bloodstream predominates;
-
vagotonic with significant dilation of arterioles and arteriovenous anastomoses and blood deposition in the capillary bed;
-
paralytic, characterized by passive dilation of capillaries, severe blood stasis in them and, as a consequence, depletion of compensatory-regulatory mechanisms.
Diagnostic
criteria.
-
Sympathicotonic collapse: usually short-term and characterized by agitation of the child, increased muscle tone, pale skin, cold extremities, tachycardia, normal or slightly elevated blood pressure, decreased diuresis.
-
Vagotonic collapse is accompanied by inhibition of the child, hypo- or adynamia, decreased muscle tone, pronounced pallor and "marbling" of the skin, acrocyanosis, a sharp drop in blood pressure, a pulse of weak filling and tension, tachy- or bradycardia, shallow, noisy breathing .
-
Paralytic collapse is characterized by loss of consciousness, bluish-purple spots on the skin, falling blood pressure to critical numbers, decreased central venous pressure, filamentous pulse, bradycardia, decreased cardiac output, bradypnea, Cheyne-Stokes respiration, oliguria.
Low
blood pressure and circulatory disorders cause cerebral hypoxia, which can
provoke convulsions in children, especially at an early age. In the absence of
emergency care, there is a real threat to the patient's
life.
Emergency
aid.
Give
the child a horizontal position with his head slightly lowered. Provide fresh
air, remove tight clothing, and examine the oropharynx.
With
sympathicotonic collapse:
-
relieve peripheral spasm by intramuscular or intravenous administration (carefully, with blood pressure control): 2% solution of papaverine at a dose of 0.1 ml / year of life or 0.25% solution of droperidol at a dose of 0.05-0.1 ml/kg;
-
in the presence of neurotoxicosis, acute adrenal insufficiency, early administration of glucocorticoids is required (intramuscularly, intravenously): hydrocortisone at a dose of 4 mg/kg or prednisolone at a dose of 1-2 mg/kg is better.
In
vagotonic or paralytic collapse:
-
provide venous access to correct the volume of circulating blood with reopolyglucin, 0.9% sodium chloride solution or Ringer's solution at a rate of 10-20 ml/kg; and with a significant reduction in blood pressure – and plasma dilators (dextran-40, refortan) at a dose of 10-20 ml/kg per year of life;
-
hormonal drugs intravenously or intramuscularly: hydrocortisone at a dose of 10-20 mg/kg/day or prednisolone at a dose of 5-10 mg/kg/day, or dexamethasone at a dose of 0.3-0.6 mg/kg/days for several receptions;
-
if hypotension persists, re-inject intravenously 0.9% sodium chloride solution or Ringer's solution in a volume of 10 ml/kg, reopolyglucin in a volume of 10 ml/kg; iv - 1% solution of mezaton at a dose of 0.1 ml / year of life or iv drip - 0.2% solution of norepinephrine on glucose at a dose of 0.1 ml/year of life (50-100 ml of 5% solution). The infusion is performed with control of heart rate, blood pressure, diuresis.
If
the measures taken are ineffective, dopamine
should be injected
intravenously, starting from 3-5 μg/kg/min with constant monitoring of heart
rate and blood pressure.
Cardiopulmonary,
cerebral resuscitation if necessary.
After
providing emergency care – hospitalization in the intensive care unit for
further treatment, taking into account the causes of
collapse.