Hypertensive crisis
Hypertensive crisis (HC) is a state characterized by a sharp and significant increase in blood pressure, accompanied by clinical symptoms of functional disorder of vitally important organs (cerebral circulation, left-ventricular insufficiency, vegetative reactions) and requires urgent decrease in pressure.
In
children, there are two types of
hypertensive crisis:
-
symptoms of damage/lesions from target organs (CNS, heart, kidneys);
The
main reasons for the development of HC in children:
-
neurogenic pathology (intracranial hypertension on the background of toxicosis, intracranial injury, tumor, meningitis or meningoencephalitis);
-
systemic diseases of connective tissue;
-
endocrine diseases (pheochromocytoma, hyperthyroidism, hyperparathyroidism, Cushing's syndrome, etc.);
-
primary arterial hypertension;
-
neuroses, psychogenic and neurovegetative disorders.
Diagnostic
criteria:
-
sudden violation of the general condition of the child;
-
severe headache mainly in the temporal-frontal and occipital areas, heaviness in the occipital region, pulsation in the temples;
-
possible dizziness;
-
visual impairment (blurred vision, floaters, loss of vision, diplopia) or hearing (tinnitus), possible visual and auditory hallucinations; objectively – a violation of the eyeballs movement; during ophthalmoscopy – narrowing of the arteries and veins of the retina, the presence of exudates, edema of the optic disc, hemorrhage on the fundus;
-
nausea, vomiting that is not related to food intake and does not bring relief;
-
paleness or redness of the face, a feeling of blood flow to the face, cold sweat;
-
weakness or irritability;
-
altered mentation, paresthesia, paresis, hand tremor, feelings of fear and anxiety;
-
possible cardialgia, chest discomfort, dyspnea, intense pulse, tachycardia;
-
blood pressure is high, exceeds the 99th percentile.
Table.
The following values of BP are typical of a hypertensive
crisis:
|
For
children under 1 year:
systolic BP (SBP) >
diastolic BP (DBP) >
|
|
For
children 1-9 years:
SBP > |
|
For
children 10-12 years:
SBP > |
|
For
children older than 12 years:
SBP > |
On
the rise of the attack, the heart tones are amplified, further weakened, a third
tone appears at the apex of the heart, the accent of the second tone appears or
increases above the aorta, a systolic murmur is heard at the apex of the heart
and aorta. Against the background of a hypertensive crisis, severe heart rhythm
disorders and signs of heart failure may occur.
The
ECG makes it possible to verify arrhythmia, signs of ischemia, myocardial
hypertrophy, overload mainly of the left heart. Significant diagnostic tests in
hypertensive crisis are X-ray examination of the abdominal cavity and
echocardiographic examination, assessment of renal and neurological
status.
Depending on the presence or absence of damage to target organs, there are: complicated and uncomplicated crises.
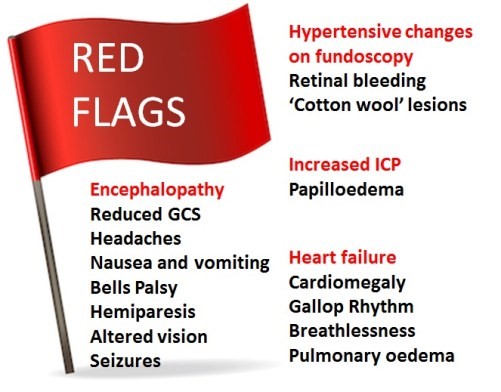
Figure. Red flags of hypertension
The principal goal of management is to gradually reduce BP and prevent end-organ dysfunction. In children and adolescents diagnosed with hypertensive crisis, the treatment goal with non-pharmacologic and pharmacologic therapy should be a reduction in SBP and DBP to <90th percentile and <130/80 mm Hg in adolescents ≥13 years of age. The rate of BP reduction should be 25% over a period of 6–8 h, which is gradually reduced to normal over 24–72 h since sudden, drastic reductions in blood pressure can itself contribute to organ damage secondary to ischemia.
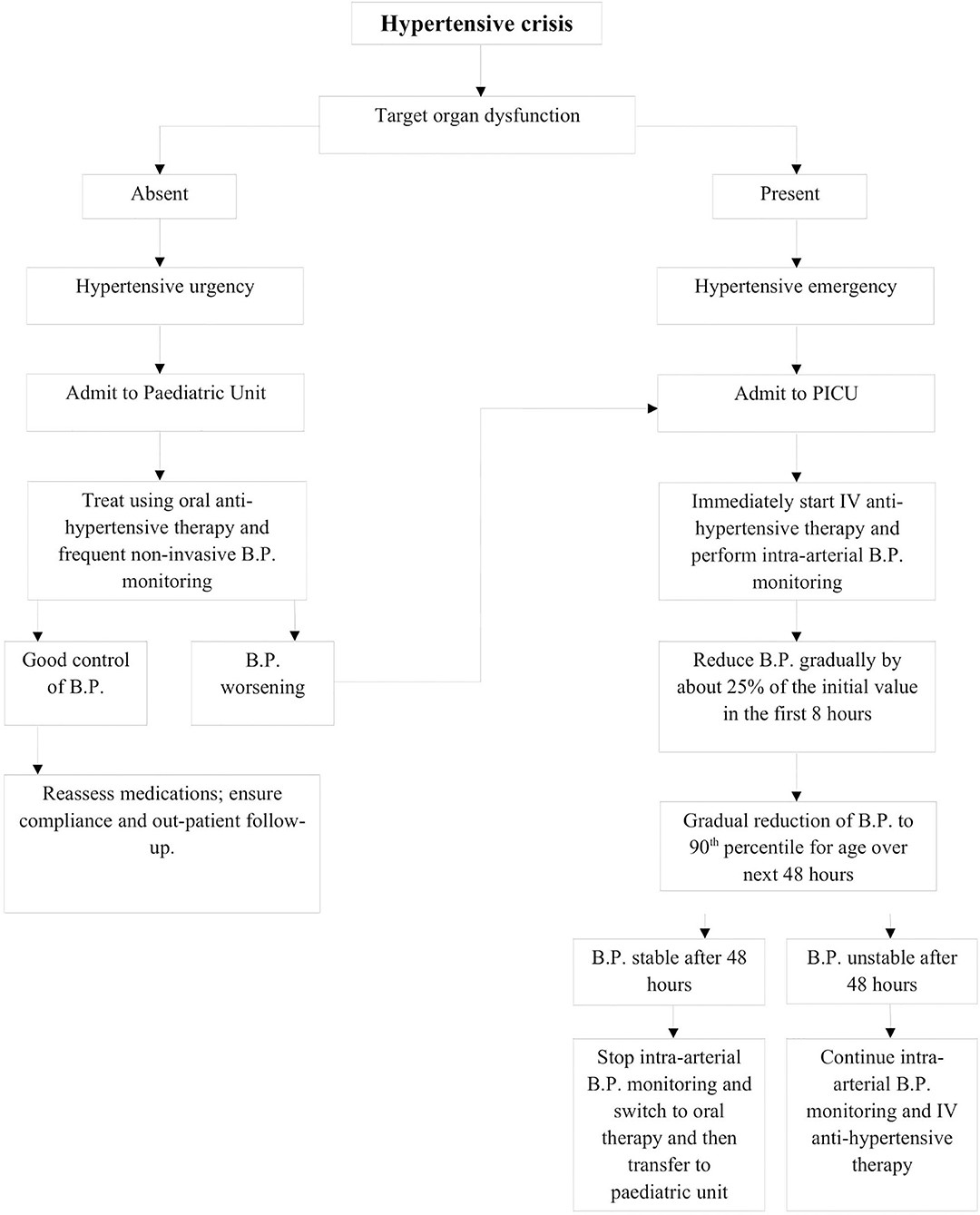
Figure . Management outline for hypertensive crisis
Emergency
care for uncomplicated HC
-
Position of the patient – on his back with his head raised.
-
Release the patient from tight clothing, ensure permeability of the upper respiratory tract.
-
Provide access to fresh air, if necessary – oxygen support.
-
At uncomplicated crisis, antihypertensive drugs are administered sublingually/orally.
Reassure
the patient. At excitement and the expressed neurovegetative
symptomatology
injection of
diazepam
(seduxen, relanium, sibazon) of 0.2-0.3 mg/kg of body weight of 0.5% of
solution intramuscularly (IM) or intravenously (IV) on 10% solution of glucose
is possible.
In
the initial therapy of HC ACE
inhibitors are used, for example, captoprilum
begins to act after 15 minutes
(due to the rapid absorption in the stomach), and the peak of action occurs
after 30-40 minutes after admission. Doses: up to 2 years 0.01-1 mg/kg/day
orally, repeated doses after 8 hours; older than 2 years from 0.5 to 6 mg/kg of
weight a day orally or sublingually in 8 hours.
Contraindications
to the prescription of captoprilum: stenosis of the renal arteries, aorta,
primary hyperaldosteronism.
Enalapril
–
dose 0.08-0.6 mg/kg/day, interval after 12-24 hours. Onset of action after 15-30
minutes, duration of action – 6 hours.
In
cases of uncomplicated HC older than 14 years, the initial use of a class II
calcium antagonist – nifedipine
sublingually at a dose of
10-20 mg is effective. The drug reduces the total peripheral resistance,
increases cardiac output and renal blood flow. Onset of action in 15-30
minutes.
In
cases of HC
with tachycardia,
beta-blockers are appropriate – propranolol
(1-4 mg/kg/day orally, after
6-12 hours). Contraindications –bradycardia, bronchoconstriction. Onset of
action after 30-60 minutes.
It
is possible to prescribe cardioselective beta-blockers – atenolol
(0.5-2 mg/kg/day in 1-2 doses)
or metoprolol
(1-6 mg/kg/day in 1 dose).
Children of early puberty should be restricted to prescribing due to the
effect on the
central regulatory structures involved in
puberty.
In
cases of aggravating
anamnesis
with uncomplicated HC,
furosemide
is used at a dose of 1-2 mg/kg
IM, daily dose up to 6 mg/kg, interval of repeated injections is 4-12
hours.
As an additional means, IV administration of 25% solution of magnesium sulfate at a dose of 0.2 ml/kg (IV bolus), seldom 2% of euphyllin 1-3 mg/kg (IV bolus), in saline.
Emergency
care for complicated HC
-
Urgent hospitalization.
-
Ensure permeability of the upper respiratory tract, if necessary, adjust ventilation, oxygen supply.
-
The method of administration of drugs is mainly IV.
-
If it is not possible to perform an IV infusion immediately before it is started, you can use sublingual or orally of one of the following drugs: older than 14 years sublingually nifedipine at a dose of 10-20 mg; captoprilum older than 2 years 0.5-1.0 mg/kg body weight; propranolol 1-2 mg/kg, clonidine – 0.002-0.03 mg/kg/day (mostly in adolescence).
-
Intramuscular injection of furosemide is possible.
-
Intravenous administration ("step-by-step", depending on the effectiveness of the previous drug):
ü
Furosemide
at a dose of 1-2 mg/kg, daily dose up to 6 mg/kg body weight, interval of
administration 4-12 hours.
ü
Selective
blocker of calcium channels of the I class – verapamil
2-10 mg/kg/days; with HC on
the background of arrhythmogenic
cardiac syndrome;
but do not use in patients with heart failure and those treated with
beta-blockers.
ü
Enalapril
0.08-0.6 mg/kg body weight per day, mainly in adolescence (effective
in acute left ventricular failure).
At
convulsions, eclampsia
25% solution of magnesium sulfate from 0.2 ml/kg to
bolus doses – 5-20 ml slowly.
In
the absence of effect
– clonidine
0.01% solution (selective
agonist of postsynaptic α2-adrenoreceptors of adrenergic neurons) – IM or
subcutaneously, at a dose of 0.3-0.5-1.0 ml. IV administration in the same doses
per 10-20 ml of 0.9% sodium hydrochloride solution slowly for 5-7-10 minutes, if
necessary – drip (at a rate of 20 drops per
minute).
In
case of vegetative disorders
use sedatives orally or IM/IV
injections diazepam (seduxen, relanium, sibazon) at a dose
of up to 0.2–03 mg/kg.
In
case of HC complication by stroke,
transient ischemic attack,
emergency care begins with the injection of enalapril 0.625-1.25
mg.
In
acute coronary syndrome,
nitroglycerin
is administered intravenously
at 2–10 mg/min, dropwise or in aerosol 0.4–0.8 mg by inhalation; enalapril 0.625-1.25 mg,
morphine
10 mg
intravenously.
In
case of pulmonary edema,
it is advisable to provide emergency care to begin with the introduction of: enalapril 0.625-1.25 mg IV; nitroglycerin IV 2-10 mg/min in drop or
in aerosol 0.4-0.8 mg by inhalation; morphine 10 mg intravenously; furasemide 20-100 mg
IV.
With
a dissecting aortic aneurysm:
propranolol
1-3
mg or verapamil
5 mg IV slowly; then – nitroglycerin
IV 2-10 mg/min drip; morphine – 10
mg IV.
In
eclampsia, preeclampsia:
cormagnesin
10%
or 20% (magnesium sulfate) 1000-2500 mg IV slowly for 7-10
minutes.
In the presence of pheochromocytoma, the alpha1-adrenoblocker prazosin 0.005–0.5 mg/kg/day is available (repeated administration in 6-8 hours).
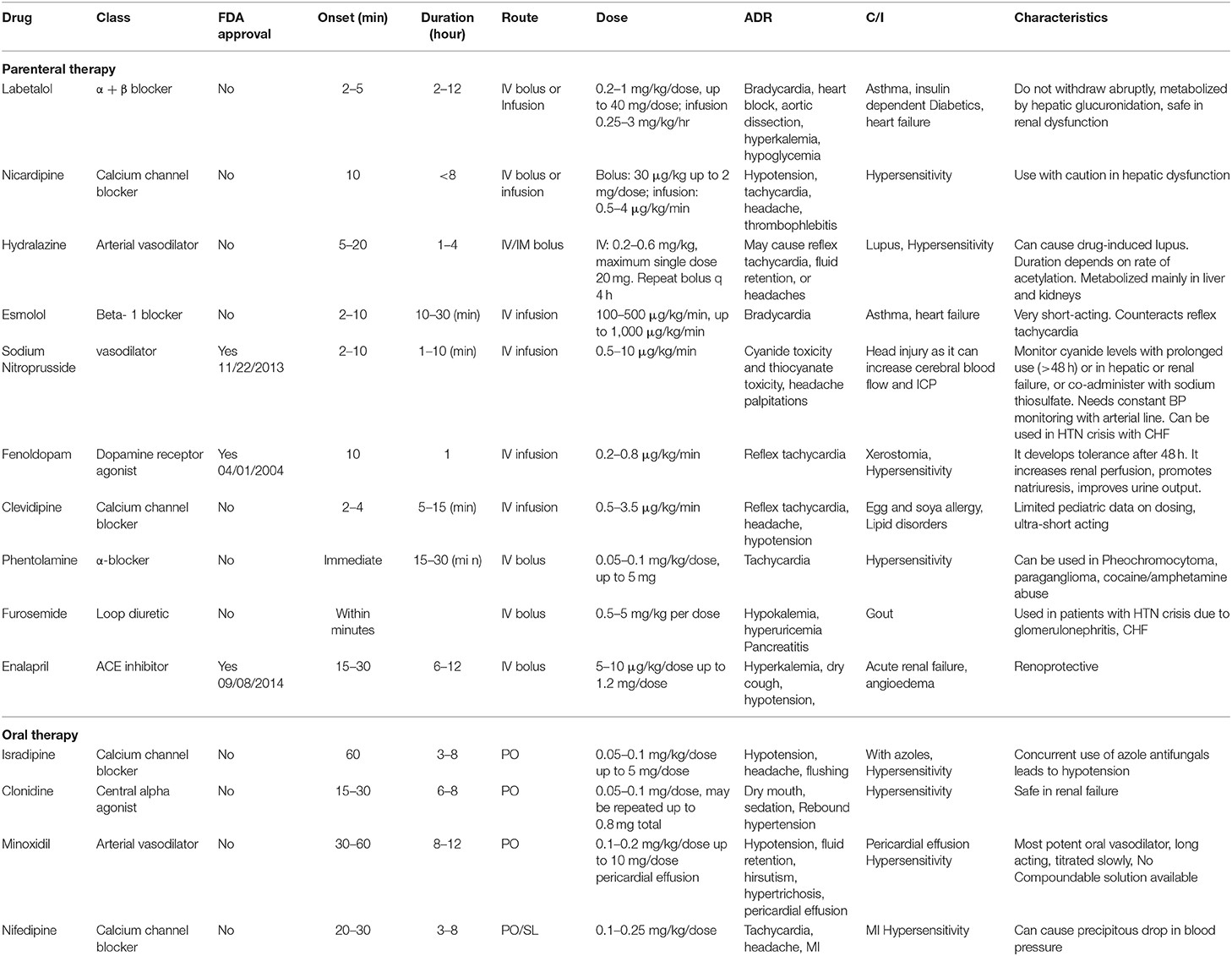
Table
. Characteristics of medications for management of hypertensive
crisis