Status asthmaticus
Status asthmaticus is a syndrome of acute progressive respiratory failure, which develops as the most threatening complication of asthma (Video) due to airway obstruction with complete resistance of the patient to therapy with bronchodilators.
Video. Pediatric asthma
The
main pathogenic factors (Video)
are:
-
deep blockade of beta-blockers, the predominance of alpha-blockers, cause bronchospasm;
-
severe glucocorticoid deficiency, which increases the blockade of beta-2-adrenoceptors;
-
inflammatory bronchial obstruction of infectious or allergic origin;
-
suppression of the cough reflex, natural mechanisms of drainage of the bronchi and respiratory center;
-
predominance of cholinergic bronchoobstruction;
-
expiratory collapse of small and medium bronchi.
Video. Asthma
pathogenic
factors
Initially, asthmatic status is characterized (Video) by relative compensation, when there are no pronounced violations of pulmonary ventilation. There is a prolonged dyspnea. An asthma attack is characterized by difficulty in exhaling while maintaining the breath. The ratio of inhalation and exhalation is 1:2, 1:2.5. Characteristic shortness of breath, moderate diffuse cyanosis, bronchospasm, stagnation in the lungs, hyperventilation, disorders of the acid-base state and gas composition of the blood. Cough is unproductive. Sputum is poorly excreted. Auscultation is determined by hard breathing with the presence of wheezing of various calibers. Breathing is performed in all parts of the lungs. The normal "ventilation / perfusion" ratio is violated. Peak expiratory rate decreases to 50-80% of normal. Pulmonary emphysema increases. Due to this, the heart tones are muted. There is tachycardia, hypertension. There are signs of general dehydration. In general, this stage is characterized by hyperventilation, hypocapnia and moderate hypoxemia. Alveolar ventilation is less than 4 l/min. Respiratory rate is more than 26 per minute. SaO2>90% at FiO2 = 0.3. Sympathomimetic and bronchodilator drugs do not relieve asthma attacks.
Video.
Asthmatic
status
In
the future, status asthmaticus is characterized by an increase in obstructive
ventilation disorders and the development of respiratory decompensation. There
is a pronounced bronchospasm with severely difficult exhalation. The work of the
respiratory muscles is inefficient (even due to hyperventilation) and is not
able to prevent the development of hypoxia and hypercapnia.
The peak expiratory rate is
less than 50% of the proper value. Motor arousal turns into a drowsy state. The
development of muscle twitching and seizures is possible. Breathing is noisy,
frequent (more than 30 per minute). Respiratory noises can be heard at a
distance of several meters. During
auscultation
number of rales decreases, in some areas of the lungs there is no breathing
(areas of "silent lung").
Total pulmonary obstruction may occur. Sputum is not separated. Tachycardia over
110-120 per minute. Alveolar ventilation <3.5 l / min. SaO2> 90% at FiO2 =
0.6. There is a pronounced dehydration of the body. As the disorders progress,
hyperventilation is replaced by hypoventilation.
The
terminal stage of asthmatic status can be called the stage of hypoxic /
hypercapnic coma. Pupils dilated sharply, the reaction to light is sluggish.
Breathing is arrhythmic, shallow. Respiration rate is more than 40-60 per minute
(may go into bradypnea). There is an extreme degree of hypoxia with pronounced
hypercapnia. SaO2 <90% at FiO2 = 1.0. Total bronchospasm and bronchial
obstruction with viscous mucus develop. During
auscultation
noises over the lungs are not heard ("dumb lung").
There is decompensation of cardiac activity, which leads to asystole and
ventricular fibrillation.
Stage
I of status asthmaticus is
the stage of relative compensation, formed as a result of resistance to
sympathomimetics.
-
Frequent occurrence of prolonged attacks of asthma during the day, between attacks of breathing is not fully restored.
-
Paroxysmal, painful, dry cough with sputum that is difficult to pass.
-
Forced position (orthopnea), accelerated breathing (up to 40 in 1 min.) with the participation of auxiliary respiratory muscles.
-
Breathing noises and dry wheezing can be heard in the distance.
-
Severe cyanosis, pale skin and visible mucous membranes.
-
At percussion of the lungs – box sound (emphysema of the lungs), auscultation – "mosaic" breathing: in the lower lungs is not heard, in the upper – hard with a moderate amount of dry rales.
-
As to the cardiovascular system – tachycardia up to 120 per minute, arrhythmias, heart pain, normal or elevated blood pressure, as a manifestation of right ventricular failure – swelling of the jugular veins and enlarged liver.
-
Signs of central nervous system dysfunction - irritability, agitation, sometimes delirium, hallucinations.
-
General blood test: polycythemia.
-
Biochemical analysis of blood: increase in the level of α1- and ɣ-globulins, fibrinogen, siromucoids, sialic acids.
-
Gas composition of blood: moderate arterial hypoxemia (РаО2 60-70 mm Hg) and normocapnia (РаСО2 35-45 mm Hg).
-
ECG: signs of overload of the right atrium, right ventricle, deviation of the electrical axis of the heart to the right.
Stage
II of status asthmaticus –
stage
of decompensation, "silent lung", progressive ventilation
disorders).
-
Extremely serious condition of patients.
-
Sharply pronounced shortness of breath, shallow breathing, the patient "catches his breath."
-
The position is forced, orthopnea.
-
The jugular veins are swollen.
-
The skin is pale gray, moist.
-
Periodically there is excitement, which is replaced by indifference.
-
At auscultation of lungs – over all surface of lungs or on a big site of both lungs respiratory noises ("dumb lung", obturation of bronchioles and bronchial tubes) are not listened, only on a small site a small amount of rales can be heard.
-
Cardiovascular system – pulse becomes more frequent (up to 140 per minute), weak filling, arrhythmias, hypotension, deaf heart tones, possible gallop rhythm.
-
General and biochemical blood tests: the data are the same as in stage I.
-
Study of blood gas composition – severe arterial hypoxemia (РаО2 50-60 mm Hg) and hypercapnia (РаСО2 50-70 mm Hg or more).
-
Research of acid-base balance – respiratory acidosis.
-
ECG: signs of overload of the right atrium and right ventricle, diffuse decrease in the amplitude of the T wave, various arrhythmias.
Stage
III of status asthmaticus –
hypercapnic
coma.
-
Unconscious patient, convulsions are possible before loss of consciousness.
-
Spilled diffuse "red" cyanosis, cold sweat.
-
At auscultation of lungs: absence of respiratory noises or their sharp weakening.
-
Cardiovascular system: pulse filamentous, arrhythmic, blood pressure is sharply reduced or undetectable, collapse, deaf heart sounds, often gallop rhythm, possible ventricular fibrillation.
-
General and biochemical blood tests: the data are the same as in stage I. Significant increase in hematocrit.
-
Examination of blood gas composition – severe arterial hypoxemia (РаО2 40-55 mm Hg) and severe hypercapnia (РаСО2 80-90 mm Hg)
Emergency
care/aid.
Emergency
care for status asthmaticus primarily includes oxygen therapy, restoration of
airway patency, elimination of hypovolemia, control of inflammation and edema of
the bronchial mucosa, stimulation of beta-adrenergic
receptors.
Oxygen therapy
with humidified oxygen 3-5
l/min, which maintains its concentration in the inhaled mixture in the range of
30-40% is indicated for all patients with a prolonged asthma attack and status.
Higher concentrations are impractical because hyperoxygenation can lead to
respiratory depression.
Infusion
therapy.
Its purpose is to fill the deficit of circulating blood volume and extracellular
fluid, which allows to normalize hemodynamics and reduce bronchial obstruction
by improving the rehabilitation of the tracheobronchial tree (sputum thinning,
etc.). Catheterization of one of the central veins is desirable for infusion
therapy and control of central hemodynamics. It should be remembered that
patients with asthmatic status are at increased risk of pleural damage and
pneumothorax, so it is safer to catheterize the femoral or external jugular vein
at the prehospital stage.
For
rehydration 5% glucose solution, rheopolyglucin, hemodesis in combination with
protein drugs are used. The volume of the liquid entered in the first day should
make 3-4 l (including food and drink). Subsequently, the liquid is injected at a
rate of 1.6 l / m2 of body surface. It is recommended heparinization
of solutions at the rate of
2.5-5 thousand units per 500 ml. The use of 0.9% sodium chloride solution in
asthmatic status is not recommended, as it may increase the swelling of the
bronchial mucosa. Administration of sodium bicarbonate solutions is indicated in
stage II-III of asthma status or laboratory-confirmed decompensated metabolic
acidosis (stage I of asthma status is usually accompanied by subcompensated
metabolic acidosis in combination with compensated respiratory
alkalosis).
The
adequacy of the infusion therapy is assessed by changes in central venous
pressure and diuresis (urinary rate with adequate infusion therapy should be
about 80 ml/h without the use of
diuretics).
Adrenoceptor stimulants
are
used in the treatment of asthma attacks. These drugs cause relaxation of the
bronchi with their subsequent expansion, have a mucokinetic effect, reduce the
viscosity of sputum, reduce mucosal edema and increase the contractility of the
diaphragm. During the development of asthmatic status, short-acting drugs are
used, which allows you to adjust the dose depending on the effect obtained. It
is shown to start treatment with selective beta-2-agonists,
as non-selective adrenoceptor stimulants cause tachycardia, increased cardiac
output and increased myocardial oxygen demand.
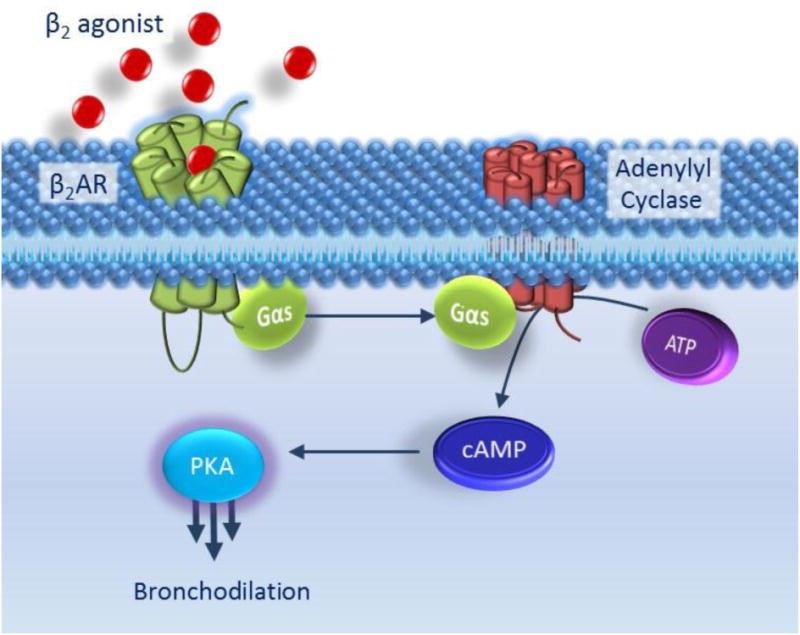
Figure
(Charlotte
K. Billington,
2017).
The
classic β2AR
signalling pathway.
|
Binding
of β2-agonist to β2AR induces a conformational
change allowing the α-subunit of the G-protein to dissociate and bind to
adenylyl cyclase. Adenylyl cyclase is thus activated and catalyses the
formation of cyclic AMP (cAMP) from ATP. cAMP molecules bind to PKA which
induces the dissociation of the catalytic and regulatory subunitsfrom each
other. Once released, the PKA catalytic subunits phosphorylate and hence
activate myriad cellular targets which results in airway smooth muscle
relaxation and hence
bronchodilation. |
Therapy begins with inhalation of salbutamol solution through a nebulizer. Repeated inhalations are indicated every 20 minutes for 1 hour. The advantage of drug administration by nebulizer therapy is the possibility of inhalation of higher doses of drugs in comparison with aerosol metered or powder inhalers (turbuhaler, diskhaler, cyclohaler, etc.).
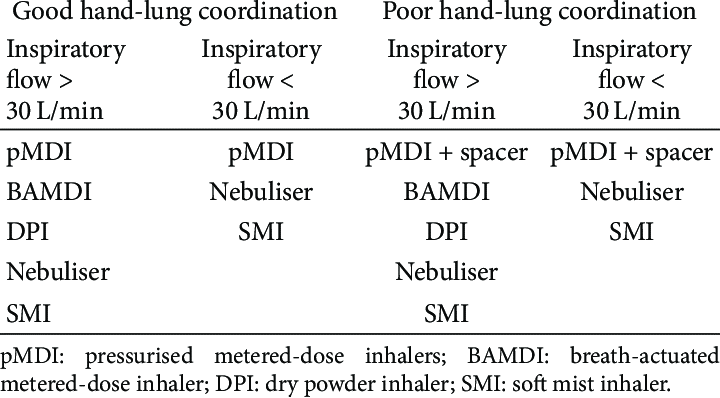
Figure (Modified from Chapman et al.). Choice of inhaler devices according to the patient's inspiratory flow and ability to coordinate inhaler actuation and inhalation.
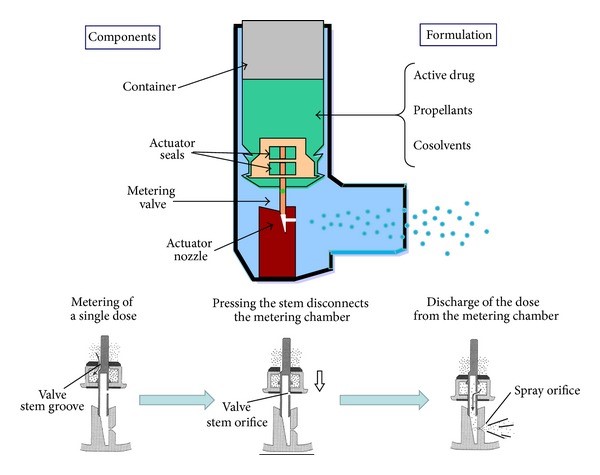
Figure.
Components of a pressurised metered-dose inhaler. Lower panels illustrate the
process of aerosol generation.
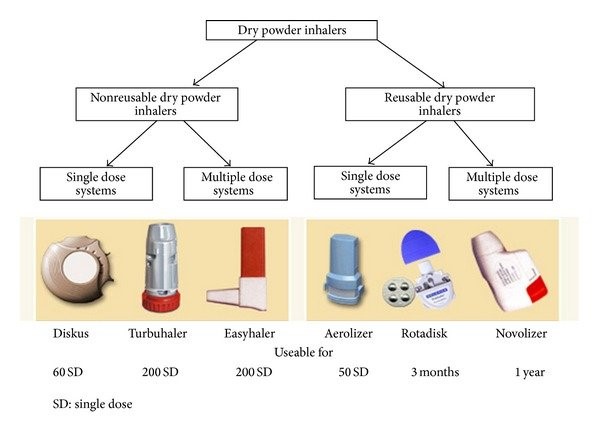
Figure. Examples of dry powder inhalers.
It
is advisable to combine beta-2-adrenomimetics with cholinolytics. A combination
of salbutamol and ipratropium bromide (Atrovent) gives a good effect. Salbutamol
(Ventolin) is a selective beta-2-adrenoceptor agonist used as a first-line drug.
Its effect occurs in 4-5 minutes, reaching a maximum of 40-60 minutes. Duration
of action about 4-5 hours. For inhalation using a nebulizer
1-2 nebula (2.5-5 mg of
salbutamol
sulfate in 2.5 ml of 0.9%
NaCl) in undiluted form is placed in a nebulizer and inhale the mixture. The
drug can also be used in the form of a metered aerosol inhaler. Berotek is also
a selective beta-2-adrenoceptor agonist. Its effect develops in 3-4 minutes with
reaching the maximum effect in the 45th minute. Duration of action is about 5-6
hours. It can be used with a nebulizer (inhalation of 0.5-1.5 ml of a solution
of Fenoterol in saline for 5-10
minutes with repeated inhalations of the same dose every 20 minutes) or as a
metered-dose aerosol inhaler.
Atrovent
(ipratropium bromide)
is an anticholinergic agent. Usually it used in case of ineffectiveness of
beta-2-agonists or in combination with them to enhance the bronchodilator
effect. The drug can be administered through a nebulizer of 0.25-0.5 mg or by
using a metered dose aerosol inhaler and spacer.
Lack
of response to adrenomimetics indicates the development of resistance of
beta-adrenergic receptors to sympathomimetics, which makes their use
inappropriate (in asthmatic status, the use of adrenergic stimulants can lead to
the development of rebound syndrome –
deterioration caused by accumulation of adrenostimulatory metabolism in the
blood).
As
to the drugs with bronchodilator action, the use of euphyllin (theophylline,
aminophylline) is shown first of all. 240 mg of the drug is administered slowly
intravenously over 20 minutes as a 2.4% solution. Then the dose is reduced to
0.5-0.6 mg / kg body weight 1 hour before the improvement of the patient's
clinical condition. The daily dose should not exceed 1.5 mg. Euphyllin inhibits
phosphodiesterase, which leads to the accumulation of adenylcyclic adenosine
monophosphatase, restoration of adrenoceptor sensitivity and removal of
bronchospasm. The drug reduces the pressure in the pulmonary artery system,
increases myocardial contractility and has a small diuretic
effect.
Glucocorticoids
suppress various mechanisms of bronchospasm and have nonspecific
anti-inflammatory and anti-edematous effects. They potentiate the effect of
bronchodilators, increasing the intracellular concentration of adenylcyclic
adenosine monophosphatase, reduce bronchial hyperreactivity and promote the
reactivation of beta-2-adrenoceptors. The initial dose is at least 30 mg of
prednisolone or 100 mg of hydrocortisone and 4 mg of dexamethasone. Next,
prednisolone is administered intravenously at a rate of 1 mg/kg/h. Other
hormonal drugs are administered in the appropriate dosage (5 mg of prednisolone
is equivalent to 0.75 mg of
dexamethasone, 15 mg of cortisone, 4 mg of triamcinolone). The intervals of
administration should not exceed 6 hours, the frequency of administration
depends on the clinical effect. On average, the treatment of stage I status
asthmaticus requires the introduction of 200-400 mg of prednisolone (up to 1500
mg/day). At the status asthmaticus of the II-III stage the dose of prednisolone
makes 2000-3000 mg/days.
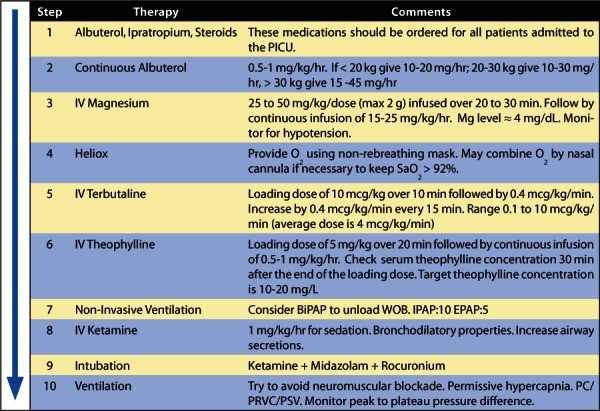
Figure 5. Severe acute asthma stepwise approach for escalating therapy.
Progression
of asthmatic status is an indication for transfer of the patient to artificial
ventilation: the appearance of signs of acute respiratory failure II-III stage
despite intensive care, increased РаСО2 and hypoxemia, progression of
symptoms of the central nervous system and the development of coma. The effect
of "overstretching" the lungs should be avoided during respiratory support, as
it threatens the development of pneumothorax. It is possible to use short-term
anesthesia, which improves the bronchodilator effect. In addition, the exclusion
of consciousness eliminates the emotional background.
The
use of antihistamines
and sedatives in status
asthmaticus is undesirable, as they may suppress breathing and cough reflex. It
is also undesirable to use diuretics, as they may worsen the existing
disturbances of water-electrolyte balance. You can use calcium antagonists,
which relax the smooth muscles of the bronchi and dilate peripheral blood
vessels, thereby balancing ventilation and pulmonary hemodynamics. In addition,
they inhibit the release of mediators from lung labrocytes and histamine from
basophils.
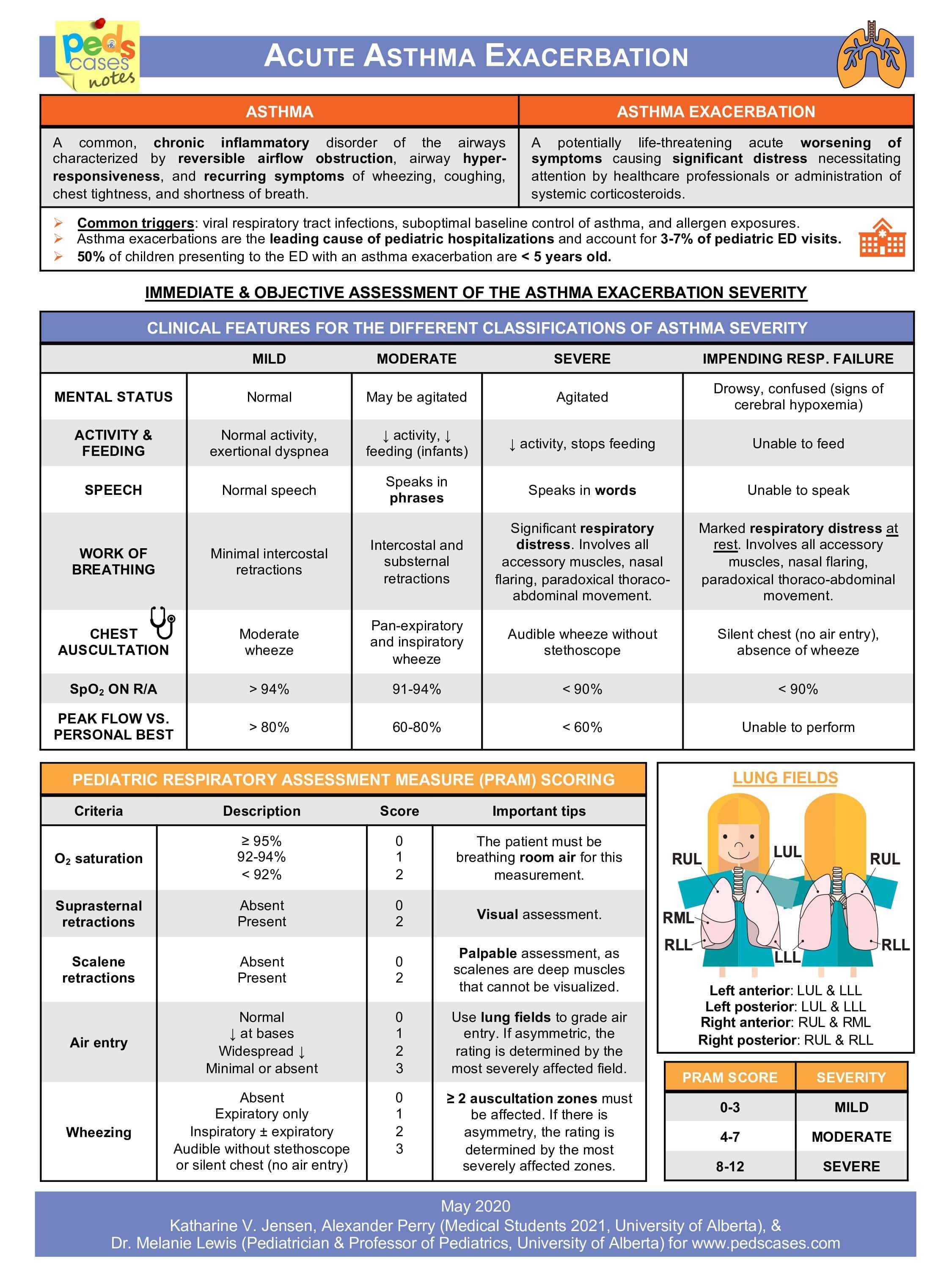
Figure. Acute asthma exacerbation
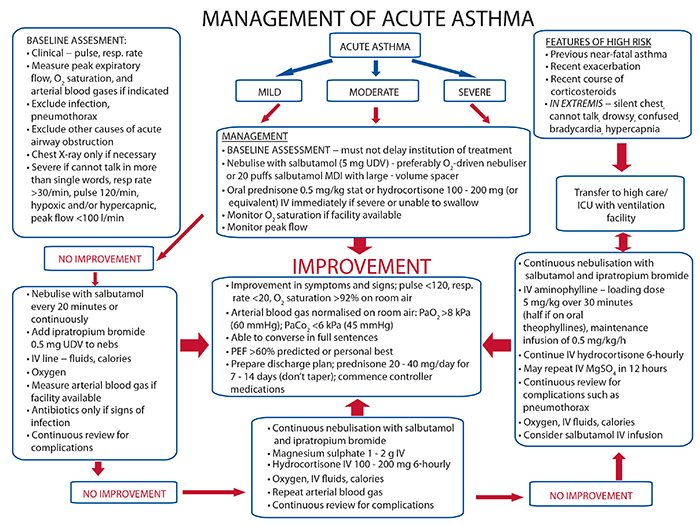
Figure.
Management of acute
asthma