Acute heart failure
Acute heart failure (AHF) – a clinical syndrome, which is characterized by a decrease in cardiac output, tissue hypoperfusion, increased pressure in pulmonary capillaries and stagnant phenomena in tissues. AHF is determined by intracardiac or extracardiac mechanisms that can pass or cause the development of clinical syndrome or irreversible lesions with the development of chronic heart failure (Video).
According
to the working classification of
AHF, there is a left ventricular (left-sided heart failure), right
ventricular (right-sided heart failure), arrhythmogenic and total heart failure.
At an early age with organic heart pathology in children, total heart failure
develops more often.
Clinical
variants of AHF:
1.
Hypokinetic
type of hemodynamics (small heart emission syndrome) –cardiogenic
shock,
characterized by arterial hypotension with signs of centralization of blood
circulation.
2.
Stagnant
type of hemodynamics:
-
right ventricular AHF (venous stagnation in a large circle of blood circulation) edema, enlargement of the liver, protrusion of cervical veins, ascites, hydrotorax;
-
left ventricular AHF (overload of a small circle of blood circulation – cardiac asthma, pulmonary edema).
3.
Hypoxic
crisis (dyspnea-cyanotic attack).
Common
causes of AHF
-
heart diseases: congenital heart disease (Video), fibroelastosis, myocardial disease, pericardial disease, exchange cardiomiopathy,myocardiodystrophy, heart tumors, etc.;
Video. Congenital heart disease
-
extracardial causes: pulmonary diseases, diseases of liver, kidney, hematopoiesis organs etc. that cause lesions or overload of myocardium.
In
addition, the main diseases and conditions that contribute to the development of
AHF can be attributed:
-
sharp decrease in the contractile capacity of myocardium due to its damage (acute myocardial infarction, myocardial ischemia, myocarditis, heart surgery, consequences of the use of artificial blood circulation, severe brain injury, toxic actions on myocardium, etc.);
-
increase of manifestations (decompensation) of chronic heart failure;
-
integrity deterioration of heart valves or cameras;
-
cardiac tamponade (Video);
Video. Cardiac tamponade
-
pronounced myocardial hypertrophy (especially with the presence of subordinate stenosis);
-
hypertensive crisis;
-
pressure increase in the pulmonary circulation (pulmonary embolism, acute pulmonary diseases, etc.);
-
tachycardia or bradycardia.
Clinical
manifestations of heart failure in children
-
symptoms of heart failure: delay in physical development, sweating, fatigue, weakness, cardiomegaly, tachycardia, changes in peripheral pulse, cold limbs, etc.;
-
symptoms of stagnation in a pulmonary circulation - tachypnea, shortness of breath, coughing, wheezing in the lungs, whistling breathing, cyanosis;
-
symptoms of stagnation in a systemic circulation - hepatomegaly, swelling of cervical veins, edema, etc.
Acute
Left Ventricular Failure
Acute
left ventricular failure is
a multifactorial disease, where the primary disorder of the heart function (left
ventricle) causes a number of hemodynamic reactions aimed at supporting blood
circulation in accordance with the needs of the body. It is the case when the
heart is unable to transfer venous flow into an adequate cardiac outlet and it
does not provide organs and tissues with the required amount of blood in the
presence of a normal or enlarged venous return.
Causes
of acute left ventricular failure:
rheumatic and non-rheumatic carditis, toxic damage to myocardium, congenital and
acquired heart diseases, arterial hypertension, cardiomyopathy, heart rhythm
disorders, heart tumors.
Clinically acute left ventricular failure is manifested by cardiac asthma syndrome and pulmonary edema.
Emergency
assistance in acute left ventricular failure
-
to control heart rate (HR), blood pressure (BP), ECG;
-
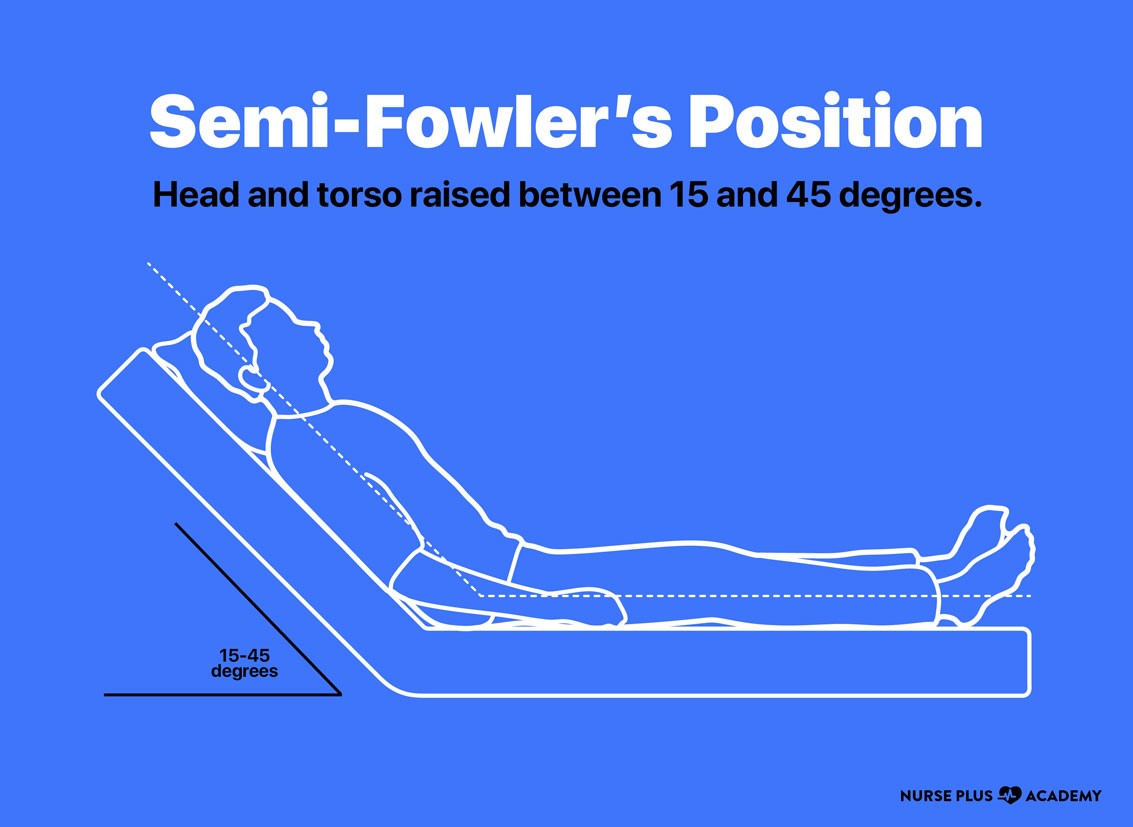
to quieten the child, let her/him lie down in semi-Fowler’s position (slightly raised the main end of the bed between 15˚ and 45˚), and in case of pulmonary edema - a sitting position with dangling legs (Figure );
-
to provide free permeability of respiratory tract, tracheobronchial sanation;
-
to maintain oxygen therapy (supplemental oxygen) with 30-40% oxygen (if possible in combination with a 10% antifomsilanum or a 30% ethanol solution) through a mask or nasal cannula, mechanical ventilation if necessary;
-
with pronounced psychoemotional excitation of the child, sedatives (diazepam (seduxen) 0,1-0,3 mg/kg iv) are prescribed;
-
with progressive pulmonary edema - 1% solution of trimeperidine (promedol) 0.05-0.1 ml/year of life or morphine (provided the absence of oppressed breathing).
In
the case of reduced BP and the hypokinetic variant of myocardial insufficiency,
cardiotonic agents are prescribed:
-
sympathomimetic amines: infusion of dopamine in an average dose of 5-10 mg/kg/min or dobutamine - 5-15 mg/kg/min by using an infusion pump in order to increase heart emission in violation of blood circulation;
-
adrenaline (epinephrine) at very low doses (0.03-0.1 mg/kg/min) should be used for children with cardiac insufficiency provided ineffectiveness of other drugs;
-
infusion therapy using a 10% glucose solution with a 4% potassium chloride solution (panangin). Daily flow of liquid is limited to 2/3 of age consumption, high-quality food;
-
cardiometabolites (potassium preparations, cocarboxylase, riboxin, L-carnitine, mildronate, etc.) to improve metabolic processes in myocardium and correction of acid-base homeostasis;
-
antimicrobial therapy (antibiotics of a wide spectrum of action iv) if necessary;
-
special treatment (correction of severe degrees of mitral stenosis, antiarrhythmic measures with arrhythmogenic form of heart failure, etc.);
-
treatment of the main disease, which led to the development of acute left ventricular failure.
Acute
Right
Ventricular
Failure
Acute
Right
Ventricular
Failure
is
a pathological condition due to a sharp decrease in the operating capacity of
the right parts of heart, which leads to a redistribution of circulating blood
volume in a systemic circulation. It
is the result of a sudden reduction of blood flow in the lungs against the
background of various diseases and pathological conditions (congenital heart
failures, bronchial asthma attacks, pulmonary artery thromboembolism, lung atelectasis, foreign body of
bronchi, hydrotorax, etc.).
Emergency
assistance in acute right ventricular failure:
-
to clarify and quick eliminate the reason that caused the development of a violent AHF (pneumothorax, obstructive lung disease, a foreign body in the respiratory tract);
-
to come down the child, let her/him lie down in bed with a slightly raised position of a head and dangling legs;
-
to provide fresh air access, to carry out inhalation of 40-50% oxygen, mechanical ventilation if necessary;
-
to control HR, BP, ECG, diuresis;
-
loop diuretics – furosemide (lasix) 1% solution iv slowly by a dose 1-2 mg/kg;
-
with pulmonary embolism - heparin at a dose of 100-400 U/kg/day IV divided into 4-6 doses or fraxiparin 225 U/kg under the control of coagulogram and fibrinolytic agents (streptokinase in older children IV drip at a dose of 100 000 U dissolved in 50 ml of isotonic solution of NaCl), embolectomy;
-
with arterial hypotension - dextran (rheopolyglucin) or its analogues at a dose of 5-10 ml/kg, IV inject slowly or drip; cardiotropic drugs (dopamine or dobutamine in the above doses);
-
correction of acid-base balance and water-electrolyte balance;
-
extremely careful use of peripheral vasodilators (nitroglycerin or sodium nitroprusside IV drip) in the intensive care unit;
-
in case of pain and significant psychomotor excitation/agitation, inject 1% solution of promedol at a dose of 0.1-0.2 mg/kg (children over 2 years);
-
with congenital cardiac malformations with reduced pulmonary circulation - myotropic antispasmodics (drotaverine, atropine) and beta-blockers propranolol (anaprilin);
-
specific treatment aimed at treating the main disease complicated by the development of acute right ventricular heart failure: immediate hospitalization of the patient to the intensive care unit.
Breath-cyanotic
attack (hypoxemic crisis)
Shortness of breath-cyanotic attack (hypoxemic crisis) is an attack of paroxysmal shortness of breath with severe cyanosis, which can be observed in children with congenital heart defects of the blue type, especially with tetralogy of Fallot (TOF). The onset of attacks is due to spasm of the outflow tract of the right ventricle and a decrease in pulmonary circulation, as a result of which a significant portion of venous blood due to a ventricular septal defect enters the aorta and progresses to hypoxemia of the systemic circulation.
Emergency
care in case of breath-cyanotic attack (hypoxemic
crisis)
-
to calm down the child, put him/her on his stomach in a knee-elbow position (with his legs pressed to his chest and bent at the knees);
-
to carry out oxygen therapy;
In
case of a severe attack of hypoxemic crisis, provide venous access and make
prescriptions/administer:
-
4.2% solution of sodium bicarbonate in order to eliminate metabolic acidosis (in a dose of 2-5 ml/kg/IV slowly for 5 minutes, if necessary, re-injection in half dose is possible after 30 minutes under the control of pH of blood);
-
promedol 1% solution at a dose of 0.1 ml/year of life or morphine (in the absence of respiratory depression);
-
in the absence of effect - carefully inject the beta-blocker propranolol (anaprilin) at a dose of 0.1-0.2 mg/kg IV drip or inject slowly in 10 ml of 20% glucose solution;
-
in the presence of seizures – seduxen (diazepam) at a dose of 0.1-0.3 mg/kg or sodium oxybate at a dose of 50-100 mg/kg;
-
with the progression of the attack and the threat of hypoxic coma, mechanical ventilation and urgent palliative surgery is necessary as well as imposition of aortic-pulmonary anastomosis;