Acute renal failure
Acute
renal failure (ARF)
is a symptom complex characterized by rapid loss of homeostatic
kidney functions (Video).
Video.
Homeostatic
kidney functions
Criteria
for the diagnosis of ARF:
oligoanuria, decreased glomerular filtration rate (GFR), relative density of
urine (osmolality), increased concentrations of creatinine, urea, serum
potassium, acid-base imbalance, anemia, hypertension.
Acute kidney injury (AKI) is classified into pre-renal (60-70%), renal (25-40%), post-renal (5-10%) and arenal (<1%) causes (Figure).
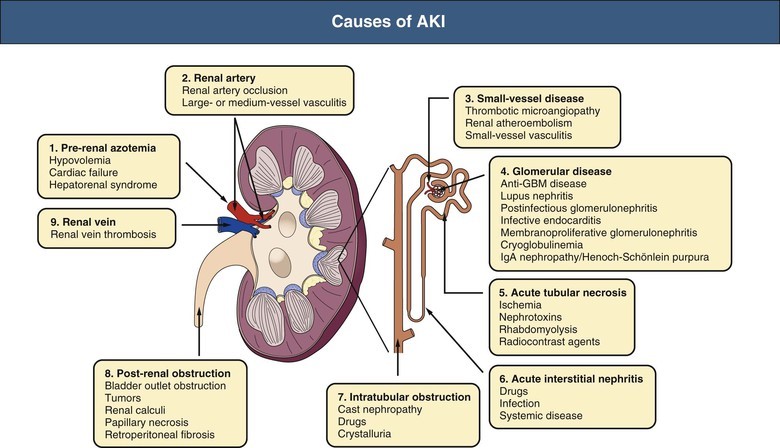
Figure
.Causes of acute kidney injury
GBM, Glomerular
basement membrane.
Functional
ARF
is a temporary impairment/disturbance of some renal functions that has a
reversible development during conservative therapy.
Organic
ARF
has no reversible development without the use of extracorporeal methods of
treatment and is characterized by a wider range of impaired renal
functions.
From
the moment of making the diagnoses (ARF) to the patient the following actions
are carried out:
-
eliminate the factor that led to the development of ARF;
-
prescribe a carbohydrate salt-free diet and special foods;
-
perform a test to restore diuresis;
-
determine the indications for dialysis;
-
apply symptomatic therapy.
Treatment
of the underlying/main disease
The
caloric diet content of patients with ARF should be 25-35 kcal/kg/day, amino
acids – up to 1.7 g/kg/day, vitamins and microelements if needed. It is
suggested to prescribe 0.8-1.0 g/kg/day of protein to patients with ARF who do
not require dialysis; 1.0-1.5 g/kg/day for ARF patients receiving renal replacement
therapy
(RRT) and up to 1.7 g/kg/day
for continuous RRT patients and for hypercatabolic patients. It is recommended
to provide food mainly by enteral administration.
The test for the restoration of diuresis is performed at BP > 60 mm
Hg., in the absence of hyperhydration
in terms of increased CBV and
decreased hematocrit and lack of urine in the bladder according to
ultrasound.
At first, an intravenous infusion of 20 ml/kg of 0.9% saline solution or 5% albumin
(human) solution
is performed for 30-60
minutes. Then a 2.4% solution of
euphyllin
is administered iv at the rate
of 1 ml/10 kg of body weight and sequentially 2-7 mg/kg of furosemide.
In the absence of urination recovery within 1.5-2 hours, re-administered
furosemide (torcemide
is
more preferable, taking into account less toxic effect on the kidneys) until the
total dose for two injections is not more than 15 mg/kg.
In the absence of a diuretic effect, titrated administration
of
dopamine
(dobutamine) is made in a
renal dose of 1.5-3.5 μg/kg/min
round-the-clock. The criterion for the adequacy of the selected dose is the
absence of hypertension. The duration of the drug administration is determined
by the initiating of dialysis. In the absence of such possibility for social or
medical reasons, the use of dopamine can be successfully continued non-stop. To
restore diuresis, it is possible to use ACE
inhibitors
and ARBs
II.
In case of impossibility of pharmacological restoration of diuresis the following indications for dialysis are determined:
Anuria
over 24 hours or oligoanuria over 3 days pH
blood less than 7.2, BE = 10 Hyperkalemia
over 6.5 mmol/l GFR<7.5 ml /min or blood creatinine over 0.4
mmol/l and/or urea over 35 mmol/l Complications
of ARF (uremic pericarditis, pulmonary edema, uncorrected hypertension,
uremic coma)
Symptomatic
therapy.
The initial stage of ARF. The prescription of renal doses of dopamine
(1.5-2.5 μg/kg/min) is evident only in the first day.
Hypovolemia,
shock:
CBV recovery (10% glucose solution, 0.9% saline
solution
according
to generally accepted principles). Stimulation of diuresis – 15% solution
of mannitol 0.2-0.4 g/kg (dry matter) iv drip.
In the absence of diuresis increase after administration of 1/2 dose, its
further administration is contraindicated, also in case of heart failure and
hypervolemia.
To
prevent hyperhydration, it is necessary to limit liquid intake (per day = loss
of perspiration 25 ml/kg + excreted urine), to restrict the injection of sodium
with food or parenterally. But 1/5 of the liquid IV – sodium
bicarbonate
solution and
in extreme cases – 0.9% saline solution.
With
normovolemia:
2% solution of furosemide
2
mg/kg, IV, if there is no increase in diuresis after 2 hours, – repeat in double
dose; in order to enhance the diuretic effect of furosemide simultaneously
iv inject titrated dopamine: 1-4.5
μg/kg/min.
Drugs
to improve renal blood flow:
2.4% solution of euphyllin – 1.0
ml/years old IV; 2% solution of trental
at
a dose of 1-2 mg/kg IV, 0.5% solution of dipiridamol – 3-5 mg/kg
IV.
Both
crystalloids and often colloids are used to restore hemodynamics.
Oligoanuric
stage of ARF. Diet: proteins are excluded, carbohydrates are given to prevent
excessive catabolism and accumulation of nitrogen metabolism. The diet is poor
in protein –10 days. Then 1 g/kg of protein is added to a
diet.
1.
The amount of liquid per day = diuresis
of the previous day + loss of perspiration + extrarenal
loss;
-
loss of perspiration 25 ml/kg/day (in newborns – 1.5 ml/kg/hour, up to 5 years – 1 ml/kg/hour);
-
external losses: defecation and vomiting –10-20 ml/kg/day, for every 10 respiratory movements > norm – 10 ml/kg/day, for every degree t > 37º – 10 ml/kg/day.
In
the presence of vomiting, 60-70% of the daily volume of liquid is given orally,
the latter intravenously. Infusion therapy is performed with glucose-saline
solutions (1/5 of the volume – rheopolyglucin).
Contraindications
with anuria: protein preparations, solutions containing potassium ions
(Ringer's solution, potassium chloride).
2.
Correction of metabolic acidosis:
-
gastric and intestinal lavage with 2% solution of soda (Na2CO3),
-
sodium bicarbonate solution IV. The dose is calculated by the formula:
|
4.2%
sodium
bicarbonate
sol. (ml) = (24 – BE) • 0.4 body weight (kg) |
It
is usually not recommended to exceed a dose of 100-200 ml per day. The rate of
injection of sodium
bicarbonate
sol. is 3 ml/kg/min. Newborns 4-5 ml/kg –
4% sodium
bicarbonate
sol., older 5-7 ml/kg –
4% sodium
bicarbonate
sol., administered very slowly + glucose –
in small doses.
3.
In case of threatening hyperkalemia
(increasing > 6 mmol/l) – IV:
-
20% glucose solution at a dose of 4-5 ml/kg with insulin 1 UNIT per 5 g of injected glucose;
4.
Treatment of complications (pulmonary and
cerebral edema)
–
osmotic laxatives (sorbitol).
5.
For
preventive measures
– antibiotics for 5 days in 1/2 dose of the average therapeutic. Nephrotoxic
antibiotics (aminoglycosides, tetracyclines, methicillin, cephalosporins of the
I generation), contraindicated sulfanilamides are not prescribed.
6.
Polyuric
stage:
the diet is enriched with salts of potassium, calcium, magnesium, sodium, but
the restriction of protein continues (increases by 0.5 g per week, but not more
than 1.5-2 g/kg). Liquid intake is not limited. When hyponatremia is less than
120 mmol/l, concentrated solution of sodium chloride is administered daily
before IV. When hypocalcemia is less than 2 mmol/l,
a 10% solution of calcium gluconate
1 ml/kg is administered daily. If azotemia persists, hemodialysis (RRT) is
continued.