Acute respiratory insufficiency/ failure
Respiratory failure
(RF) is a pathological
condition of the body in which the maintenance of normal gas composition of the
blood is not provided, or it is achieved due to the stress of the compensatory
mechanisms of external respiration.
In the development of acute respiratory insufficiency, compensatory mechanisms are included, in particular shortness of breath of inspiratory, expiratory or mixed nature with the participation of appropriate auxiliary muscles.
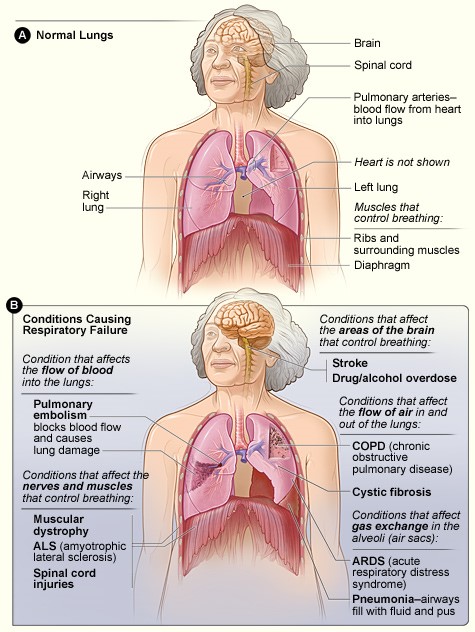
Figure.
Respiratory
failure
Types of respiratory failure
(Video)
Video. Types of respiratory failure
1. Ventilation type.
There are 3 stages of
ventilatory RF:
-
Clinical signs of ventilatory RF of the I stage/degree at a bronchoobstructive (asthmatic) syndrome – shortness of breath of expiratory character with participation of auxiliary muscles, moderate tachypnea (25–50% of age norm), absence of cyanosis (blood saturation at carrying out pulse oximetry (Video) over 90%); at groats or a foreign body of respiratory tracts – moderate tachypnea of inspiratory character, absence of cyanosis, PaCO2 of 45–55 mm of mercury.
-
At RF of the II stage/degree – shortness of breath of expiratory or inspiratory character, can be mixed character (acute bronchiolitis) with participation of auxiliary muscles. Respiration rate increases by 50-100% of the age norm, there is perioral cyanosis, tachycardia, blood saturation of about 90%, but not lower, PaCO2 56-70 mm Hg.
-
At RF of the III stage/degree - the marked/pronounced shortness of breath with participation of auxiliary muscles – Inspiratory or expiratory character (respiratory rate more than 100% of age norm), the marked/pronounced tachycardia, acrocyanosis, saturation of blood (SaO2) at carrying out pulse oximetry - less than 90%, PaCO2 Hg.
Video. Pulse
oximetry
2. Shunt-diffusion
(parenchymal).
There are 3 degrees of shunt-diffusion RF:
At
parenchymal RF, the clinical manifestations of RF of the I, II or III
stage/degree are the same, but shortness of breath is mainly inspiratory in
nature with the participation of intercostal muscles, swelling of the wings of
the nose. At III stage of RF, there is moaning breath, blood saturation is
always below 90%. The III degree of RF is an absolute indication for tracheal
intubation and ventilation. In some forms of ventilatory RF, ligamentous
stenosis of the larynx, foreign body of the airways during emergency care of the
child at the prehospital stage by doctors of linear ambulance crews one of the
main ways to restore airway patency in the development of severe RF is
cricothyrotomy between the thyroid and cricoid
cartilage).
3.
Mixed.
There are also central (in the lesion of the brain structures, responsible for respiration) and peripheral – in disorders of neuromuscular transmission at the level of synapses; primary – damage directly to the respiratory system and secondary – primary damage to another vital system (eg. cardiovascular), which then leads to acute RF.

Figure. Types of respiratory failure
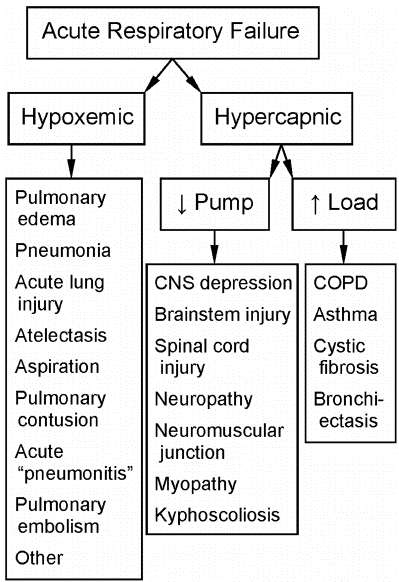
Figure. Acute respiratory failure
General
principles of therapy of respiratory failure:
-
Elimination of the cause that led to the development of RF;
-
Support of free airway patency;
-
Improving hemodynamics, microcirculation, oxygen transport from the lungs to the tissues, the function of tissue respiration, the elimination of disorders of oxygen-alkaline balance;
-
Reducing the load on the respiratory system.
Elimination
of the cause that led to the development of RF:
-
for tracheobronchial tree infections and pneumonia, antimicrobial therapy is prescribed;
-
at a pneumothorax the drainage of a pleural cavity is carried out;
-
in case of mechanical obstruction of the respiratory tract, the foreign body is removed.
Oxygen therapy
is necessary when it is
impossible for the lungs to provide normal blood oxygenation parameters
(PaO2>90 mm Hg) during air respiration (FiO2 = 0.21) and can be used for
spontaneous, artificial or auxiliary lung ventilation. The regimen of inhalation
oxygen therapy can be short-term, continuous or intermittent depending on the
severity and main physiological mechanisms of acute RI. It is also necessary to
take into account the possibility of heating (37-39°C), optimal humidification
(from 30 to 40 mg of water in 1 liter) of oxygen-air mixture with its
appropriate concentration. The percentage of oxygen in the inhaled air depends
on the method of oxygen therapy: endotracheal intubation allows to supply
through a tube of oxygen at a concentration of 100% (FiO2 = 1.0), in a tent at
an oxygen supply rate of 6-8 liters per 1 min - up to 30 % (FiO2 = 0.3), through
the nasopharyngeal catheter - up to 40% (FiO2 = 0.4), through a tightly applied
mask – up to 80% (FiO2 = 0.8), through the laryngeal mask with tamponade of the
oral cavity – about 100 % (FiO2 = 1.0).
The
optimal concentration of oxygen
in the inhaled mixture is the
minimum concentration that provides the lower allowable threshold of PaO2 (about
75 mm Hg) and SpO2 (about 95%). With marked hypoxemia, inhalation of 100% oxygen
is allowed as a short-term life-saving procedure of resuscitation measures,
although for longer use of oxygen-air mixture, the optimal concentration is
30-40%. It is necessary to consider the possibility of negative effects of
oxygen on the child's body, especially in high concentrations in case of
prolonged or improper oxygen therapy (toxic effects on the central
nervous system; negative effects on lung tissue; decreased lung
excursion, dehydration, burns of the tracheal and bronchial mucosa, retinal
detachment, retinal hemorrhage, retrolental dysplasia, especially in premature
infants, water intoxication).
Maintaining
the free passage of the airways – improving the drainage function of the
bronchi. To perform this, mucolytics are used to improve microcirculation –
teophylline
2% solution at a dose of 0.1
ml/kg for children under 1 year, 1 ml per year of life for children after one
year intravenously, warm-moist inhalation.
Improving
hemodynamics
– the use of cardiac glycosides: strophanthin
0.05% for children under 1
year in a single dose of 0.1-0.15 ml 1-2 times a day intravenously in 10%
glucose solution slowly; after 1 year – in a dose of 0.2-0.4 ml, depending on
age.
Reducing
the load on the respiratory system. Ventilation
is indicated in cases where
spontaneous breathing or previously used respiratory techniques do not provide
adequate oxygen support or removal of carbon dioxide from the
body.
-
absence of independent breathing;
-
acute respiratory disorders, pathological respiratory rhythms, agonal breathing;
-
clinical signs of increased hypoxemia and/or hypercapnia, if they are not eliminated after adequate therapy (restoration of airway patency, inhalation of oxygen, elimination of hypovolemia and metabolic disorders, analgesia if necessary).
Differentiated
indications for ventilation:
-
traumatic brain injury with signs of respiratory and consciousness disorders;
-
overdose of drugs, including sedatives;
-
chest injuries;
-
ineffective treatment of asthmatic status;
-
the presence of hypoventilation syndrome of central origin or caused by impaired neuromuscular transmission, as well as the need for muscle relaxation (epistatus, tetanus, convulsions).
Indications
for mechanical ventilation in newborns:
-
absence of independent breathing;
-
prolonged, frequent attacks of apnea;
-
severe progressive respiratory failure, cyanosis of the skin with oxygen supply> 50% in the inhaled mixture, tachypnea (> 80 per min) or bradypnea (<30 per min);
-
seizures that cannot be eliminated;
-
results of blood gas studies – PaO2 <50 mm Hg.; PaCO2> 60 or increase> 10 mm Hg. per hour; pH <7.2;
-
even in the presence of normative indicators of blood gases, but when the child's body spends a lot of effort to eliminate aerodynamic drag, with severe stridor, Pierre Robin sequence, tumors with impaired airway patency.
Acute
stenotic laryngotracheitis (croup)
is
an acute laryngotracheitis of mainly viral etiology, accompanied by laryngeal
stenosis, hoarse voice, barking cough and stridor.
There
are 4 degrees of severity of stenosis (Video):
Video. Stenosis
I
degree (compensated
stenosis). The condition is moderate, consciousness is clear. The child is
restless, periodically there is inspiratory shortness of breath, barking cough.
Hoarseness of a voice is noted. Normal color of skin. Heart rate exceeds the age
norm by 5-10%.
II
degree (subcompensated
stenosis). The condition is serious, the child is excited. Stridor breathing,
rough barking cough, inspiratory shortness of breath with involvement of a
jugular fossa and other pliable places of a thorax are characteristic. The voice
is hoarse. Paleness and cyanosis of the skin and mucous membranes are detected,
the heart rate exceeds the age norm by 10-15%.
III
degree (decompensated
stenosis). The condition is very serious. The child is excited or inhibited,
consciousness is confused. There is a sharp inspiratory dyspnea with the
participation of auxiliary muscles, exhalation is shortened. Skin and mucous
membranes are pale, earthy color, characteristic acrocyanosis, cold sweat.
Symptoms of circulatory failure are developed: marbling skin, heart rate exceeds
the norm by more than 15%, deafness of heart sounds, frequent arrhythmic pulse,
enlarged liver.
IV degree (asphyxia).
The condition is extremely
severe, there is no consciousness, the pupils are dilated, and seizures often
occur. Shallow breathing. The skin is cyanotic. A formidable sign is
bradycardia, which precedes cardiac arrest.
Emergency
aid (Video).
Emergency physicians should perform oxygen therapy to prevent hypoxia and
acidosis. If the patient has a clinic of severe RF, it is necessary to perform a
cricothyrotomy. To do this, place the child on his back with his head
outstretched (roller under his shoulders) and after treating the skin with
antiseptic and "lemon peel" local anesthetic, perform a dissection of the
membrane between the thyroid and annular cartilage and cricoid
cartilage
dilution to the sides.
Video.
Respiratory
Distress: ABC, Diagnosis & Examination
An
important differential diagnostic criterion for the difference of RF II degree
from RF III degree in the child's anxiety is the introduction of sedatives:
sodium oxybutyrate 20% – 100 mg/kg or diazepam 0.5% – 0.5 mg/kg. If the
retraction of the compliant places decreased after calming the child and medical
sleep, blood saturation is more than 90% and there is no acrocyanosis, the child
has RF II degree; the lack of effect after the introduction of sedatives and the
preservation of severe inspiratory dyspnea with subsidence of the pliable areas
of the chest indicates decompensated RF. Direct laryngoscopy and tracheal
intubation are performed, and the tube size should be 0.5 – 1 times smaller than
the age. Before transportation, the patient is administered corticosteroids
(prednisolone or dexamethasone) at a rate of 3-5 mg/kg of prednisolone. In the
presence of an inhaler, inhalation is performed with the addition of adrenaline
or other vasoconstrictor to reduce laryngeal edema. Transportation of the child
with groats should be carried out only in that hospital in which there is a
department of resuscitation and intensive care.
Bacterial epiglottitis
is
an acute bacterial lesion of the epiglottis, most commonly caused by H. influenzae type B, which rapidly
results in severe airway obstruction. It should be noted that the examination of
the throat should be performed with extreme caution due to the possibility of
complete airway obstruction. Moving the baby to a supine position can lead to
asphyxia and cardiac arrest.
Emergency
aid. A
child diagnosed with epiglottitis should be urgently hospitalized in the
intensive care unit. Orotracheal or nasotracheal intubation (Video) should be
continued as the method of choice for grade III RF. Emergency physicians (Video)
(in case of acute deficiency of time and decompensation of RF in a child) should
use conicotomy (cricothyroidomy).
It is also necessary to establish peripheral venous access for detoxification
infusion therapy with solutions of crystalloids; administration of antibiotics
(ceftriaxone
in a single dose of 40-50
mg/kg or amoxiclav
– 20-30 mg/kg); before
transportation – a single injection of corticosteroids (prednisolone)
at a dose of 3-5 mg/kg; it is necessary to carry out inhalations with humidified
oxygen and for the purpose of sedation to enter in / in 20% of
sodium oxybutyrate
of 70-100 mg/kg or 0,5% of
sibazon in a dose of 0,3-0,5 mg/kg.
Video. Demonstration of nasotracheal intubation
Video.
Types of intubation