Stokes-Adams attacks
Stokes-Adams attacks (SAA) – attacks of loss of consciousness accompanied by respiratory disorder and seizures due to a sharp decrease in cardiac output and cerebral ischemia, which occur against the background of acute cardiac arrhythmias.
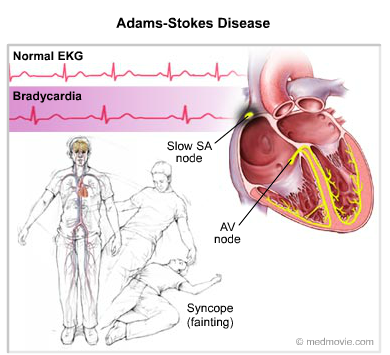
Figure . Stokes-Adams attacks
The
reasons for the development of the syndrome
are arrhythmias and violation of conduction, which lead to both an excessive
decrease (severe bradyarrhythmia) and an increase in (tachyarrhythmia) heart
rate:
At
the heart of the manifestations of SAA is the absence of cardiac output during
periods of ventricular asystole. Changes in the walls of blood vessels of the
brain, usually due to atherosclerosis, increase the risk of developing this
pathology.
SAA
on the background of decreased heart rate:
-
at AV blockade (50-60% of cases of SAA). If the complete blockade is above the AV-node ("proximal"), then the role of the rhythm driver assumes pacemaker cells of the AV connection (capable of generating about 40 pulses per minute). If lower ("distal" blockade) – impulses generate the cells of His bundle (25-30 per minute). The development of neurological symptoms usually occurs with a decrease in the frequency of ventricular contractions <30 beats/min.;
-
sick sinus syndrome (SSS) (30-40% of cases of SAA) the main rhythm driver for various reasons begins to generate pulses with inadequately low frequency.
SAA
on the background of increased heart rate:
-
with atrial flutter (up to 5% of cases of SAA), the AV node usually does not transmit pulses with a frequency of 1: 1, and the ventricles contract at a more or less acceptable rate (<150 beats/min). However, with the improvement of the conduction of the AV node (emotional or physical activity, medication) or in the presence of additional conduction pathways, each pulse begins to reach the ventricular myocardium, which leads to their frequent ineffective contractions (> 200-250 beats/min).
Emergency
assistance
On
the prehospital (hospital) stage at the development in a child with SSS severe
bradycardia with clinical signs of SAA, urgent measures are
taken:
-
Ensuring free access of air to the airways of the child;
-
Carrying out the oxygen therapy if possible;
-
Injection of atropine sulfate 0.1% IM under the root of the tongue or IV at a dose of 0.005-0.01 mg/kg or 0.05 ml/year of life. In the absence of the effect of atropine, aminophylline 2.4% solution intravenously at a dose of 2-4 mg/kg can be used.
-
Ensuring urgent hospitalization of the child to the intensive care unit.
-
To eliminate the syndrome of small cardiac output with drug therapy, the heart rate of a sick child is increased above the critical level: atropine sulfate 0.1% solution IV at a dose of 0.005-0.01 mg/kg or 0.05 ml/year of life, isoproterenol IV at a dose of 1-2 μg/(kg/min), dopamine IV at a dose of 5-8 μg/(kg/min).
-
In the absence of effect from these measures and the preservation of the syndrome of small cardiac output, signs of heart failure, recurrent SAA consultation with a cardiac surgeon is necessary to address the issue of urgent surgical implantation of an artificial pacemaker in a cardiac surgery center.