Paroxysmal tachycardia
Paroxysmal tachycardia
– an attack of sudden heart
rate > 150-160 beats per minute in older and > 200 beats per minute in
younger children, lasting from a few minutes to several hours (rarely days),
with a sudden recovery of heart rate, having specific ECG
manifestations.
Depending
on the location of the ectopic center of increased automatism or constantly
circulating re-entry wave, there are atrial, atrioventricular and ventricular
forms of paroxysmal tachycardia. The first two forms are combined into
supraventricular paroxysmal tachycardia. Given the complexity of the diagnosis
of paroxysmal arrhythmias, according to international guidelines, all
tachyarrhythmias are divided into two types:
tachycardia
with a narrow QRS complex (antegrade conduction through the AV node); most often
- supraventricular paroxysmal tachycardia;
tachycardia with a wide complex of QRS (antegrade conduction through an additional path); requires emergency differential diagnosis among different supraventricular and ventricular tachycardias. If it is impossible to completely rule out ventricular tachycardia, treatment is carried out in the same way as for proven paroxysm of ventricular tachycardia.
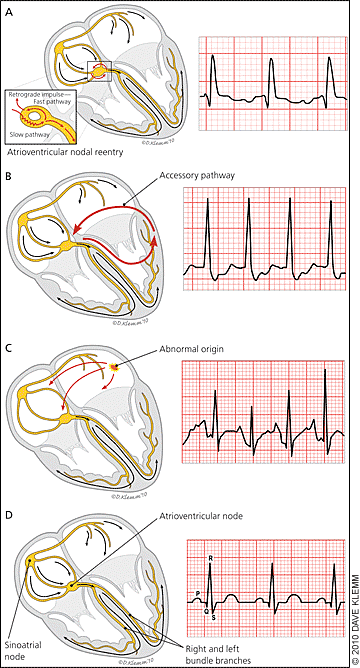
Figure.
|
(A) In
typical atrioventricular nodal reentrant tachycardia (antegrade conduction
down the slow atrioventricular nodal pathway and retrograde conduction up
the fast pathway), the retrograde P wave may not be seen or may be visible
early after the QRS complex. When visible, it often appears as a pseudo R
wave in lead V1. (B) In
atrioventricular reciprocating tachycardia, there is typically a short RP
interval, with the timing and morphology of the P wave dependent on the
site and conduction velocity of the accessory pathway. (C) Atrial
tachycardia typically produces variable RP and PR intervals because
atrioventricular conduction depends on atrioventricular nodal properties
and the tachycardia rate. In atrial tachycardia, the morphology and axis
of the P wave are influenced by atrial site of origin and tachycardia
mechanism. Short- and long-term therapies are discussed in the text. (D)Normal
sinus rhythm. |
The
main causes of paroxysmal tachycardia attack:
-
organic lesions of the heart (dystrophic, inflammatory, necrotic and sclerotic damage to the heart muscle and conduction system of the heart in acute myocardial infarction, myocarditis, cardiomyopathies, heart defects);
-
violation of autonomic regulation of heart rhythm;
-
electrolyte disturbances;
-
presence of visceral cardiac reflexes and mechanical effects (additional chords, mitral valve prolapse, adhesions);
-
psycho-emotional and physical stress.
Supraventricular paroxysmal tachycardia
(SVT)
is characterized by an increase in heart rate to 140-200 beats per minute,
sudden onset and sudden cessation/stop of the attack. The duration of the attack
lasts from a few seconds to several hours and even days. With an increase in
heart rate of more than 220-250 per minute, a small cardiac output syndrome is
developed. ECG in the atrial form of paroxysmal tachycardia registers a number
of consecutive atrial extrasystoles (not less than 4-6 with a frequency of more
than 160 per minute). The wave P of
various shapes (+, -) and / or is not defined. The QRS complex is not changed.
Incomplete AV-blockade of I-II degrees can be layered. The most informative for
diagnosis is electrophysiological examination of the conduction system of the
heart through the esophagus and daily holter monitoring.
ECG findings for common types of SVT.
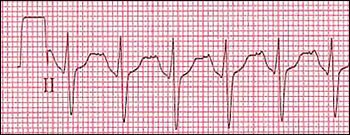
Figure.
|
Electrocardiogram
of a narrow complex tachycardia with a 1:1 atrioventricular association in
a 16-yearold girl with tachypalpitations. The differential diagnosis
includes atrial tachycardia, atrioventricular nodal reentrant tachycardia,
and orthodromic atrioventricular reciprocating tachycardia. Rhythm was
terminated with 6 mg of intravenous adenosine
(Adenocard). |

Figure.
|
Postconversion
electrocardiogram demonstrating the typical features of ventricular
preexcitation with short PR interval and prominent delta wave. This
finding supports orthodromic atrioventricular entry as the likely
mechanism of supraventricular tachycardia. Diagnostic electrophysiology
confirmed the mechanism. |

Figure.
|
Electrocardiogram of a narrow complex tachycardia with a 1:1
atrioventricular association. This example represents atrioventricular
reciprocating tachycardia, which has a high cure rate with catheter
ablation therapy. |
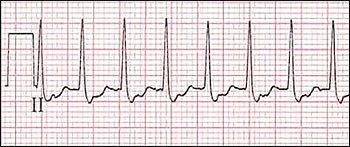
Figure.
|
Electrocardiogram
of a narrow complex tachycardia with atrioventricular association and
right bundle branch block aberration. This example represents
atrioventricular nodal reentrant
tachycardia. |
-
examination of the respiratory tract;
-
conducting (if necessary) oxygen therapy in order to achieve saturation in the range of 94-98%;
-
monitoring of vital signs and recording of 12-leads ECG;
-
providing intravenous access;
-
blood glucose testing and treatment of hypoglycemia if needed.
Tachycardia with a narrow QRS complex, regular -
stable:
-
performing vagus tests;
-
adenosine 0.1 mg/kg (maximum dose - 6 mg), in case of ineffectiveness - repeat the procedure, increasing the dose to 0.2 mg/kg (maximum 12 mg); usually 0.5-1.0 ml for preschool children and 1.0-2.0 ml for school children. In case of inefficiency, it is permissible to inject twice more with an interval of at least 2 minutes.
-
verapamil can be considered as an alternative in older children, however, it cannot be used to treat infants: verapamil 0.25% iv solution, very slowly 0.1-0.15 mg / kg (without dissolution) under blood pressure control and heart rate in a dose: up to 1 year 0.4-0.8 ml, 1-5 years 0.8-1.2 ml, 6-10 years 1.2-1.5 ml, 11-15 years 1.5 -2.0 ml. Verapamil is contraindicated in the supraventricular form of PT with aberrant (reverse) ventricular complexes, in children of the 1st year of life (development of severe hypotension), in Wolff-Parkinson-White syndrome, in AV-blockade, in sinus weakness syndrome. The drug is not prescribed simultaneously with quinidine and beta-blockers.
Tachycardia
with a narrow QRS complex, regular - unstable:
synchronized
electrical cardioversion
should be performed – 0.5-1
J/kg for the first dose; repeated doses should be 2 J/kg.
Tachycardia
with a wide QRS complex, regular - stable:
occurs in patients with premature ventricular excitation syndrome; who need
maximum care during care (typical data on the ECG monitor are shortening of the
PQ interval and, in some cases, delta waves):
-
adenosine 0.1 mg/kg (maximum dose – 12 mg) in supraventricular tachycardia with aberrations;
-
as an alternative can be used: amiodarone (Cordarone) 5 mg/kg (maximum dose - 150 mg) for 5-10 minutes, followed by a long infusion at a dose of 10 mg/kg/day or procainamide (Novocainamide);
-
the use of atrioventricular node blockers such as adenosine, calcium channel blockers (verapamil), digoxin, and beta-blockers should be avoided in patients with premature ventricular excitation syndrome (ie, Wolff-Parkinson-White syndrome and Lown-Ganong-Levine syndrome (LGL)). These drugs can cause a paradoxical increase in ventricular contractions.
Tachycardia
with a wide QRS complex, regular - unstable:
synchronized
electrical cardioversion should be performed - 0.5-1 J / kg. In the absence of
effect, it is recommended to consult a cardiac surgeon regarding the need for
pacing or electropulse therapy through the
esophagus.
Ventricular paroxysmal tachycardia.
In
ventricular paroxysmal tachycardia (VPT), the source of ectopic impulses is
located in the conductive system of the ventricles - the bundle of His, the
branches of the bundle of His or Purkinje fibers. In contrast to the
supraventricular form of SHPT, it is almost always associated with myocardial
damage.
Reasons:
-
organic myocardial damage: carditis, cardiomyopathy, heart disease, cardiosclerosis;
-
intoxication with digoxin, quinidine; hypo- and hyperkalemia, prolonged QT interval syndrome;
-
very rarely develops in vegetative-vascular dysfunction, thyrotoxicosis, psychophysical overload;
-
chronic (continuously recurrent) VPT occurs in severe hemodynamic disorders and is a life-threatening condition (transition to ventricular fibrillation and progression of circulatory failure).
VPT
is characterized by an increase in heart rate to 120-250 beats per minute,
sudden onset and sudden stop of the attack. With an increase in heart rate of
more than 120-140 beats per minute, there may be a syndrome of small cardiac
output. The ECG records "attacks" of successive ventricular extrasystoles (more
than 5) with short periods of sinus rhythm. QRS complexes are wide (more than
0.1 seconds) and deformed, T-wave are discordant (inverse) to the main wave of
the QRS complex. The P-wave is rarely recognized by layering on other elements
of the ECG. VPT can be mono- or polymorphic. Polymorphic or chaotic VPT is a
threat to the development of ventricular fibrillation.
Emergency
aid:
-
lidocaine 1% intravenously slowly for 2 minutes at a dose of 0.5-1.5 mg / kg in 10-15 ml of isotonic solution of 0.9% sodium chloride or 5% glucose solution. In the absence of effect, you can repeat the injection of lidocaine in 5-10 minutes in half dose;
-
in the absence of effect - aimalin (gilurytmal) 2.5% solution intravenously very slowly for 10.0-20.0 ml of 0.9% NaCl solution at a dose of 1 mg / kg;
-
in the absence of effect - intravenous administration of 5% solution of amiodarone (cordarone) intravenously very slowly at 10.0-20.0 ml of 5% glucose solution at a dose of 5 mg / kg;
-
in the absence of effect - consultation with a cardiac surgeon on the need for pacing or electropulse therapy through the esophagus;
-
for the prevention of thromboembolism in patients with mitral heart disease, hypertrophic cardiomyopathy, history of thromboembolism before and after routine electrical cardioversion for 2-3 weeks, prescribe indirect anticoagulants;
-
in the presence of an additional source of tachycardia, after electrophysiological examination, the method of radiofrequency catheter ablation is used. In the absence of effectiveness of conservative therapy, implantation of a cardioverter-defibrillator is performed;
-
etiopathogenetic therapy of the main heart disease;
-
according to the indications of neurotropic drugs;
-
cardiac glycosides in ventricular paroxysmal tachycardia are contraindicated.